Understanding Posterior Tibial Tendinopathy
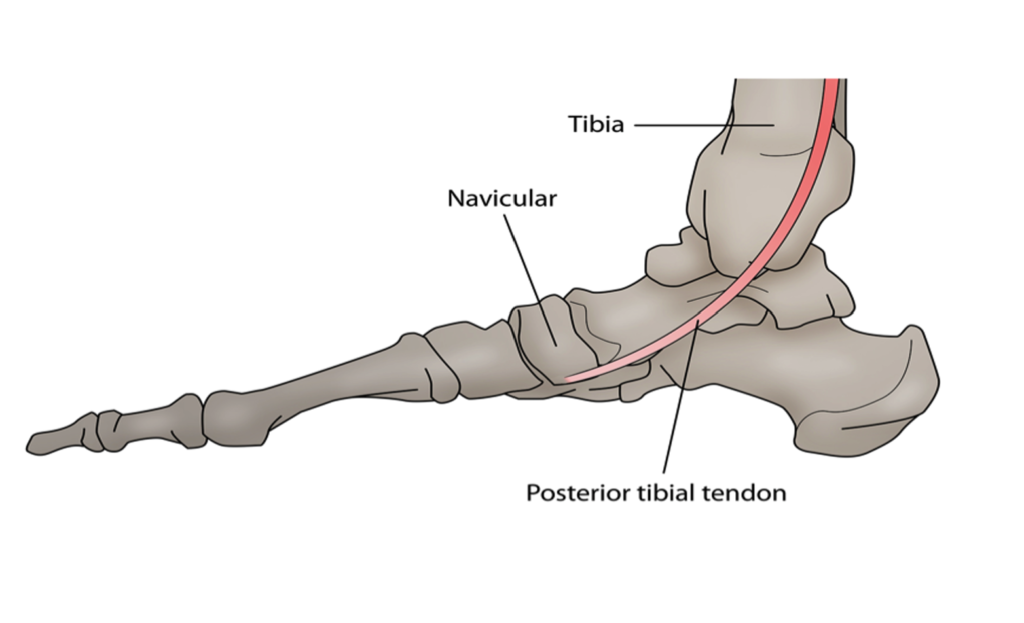
Posterior Tibial Tendinopathy (PTT) is a common condition that affects the posterior tibial tendon, a crucial structure in the lower leg responsible for maintaining the arch of the foot and providing support during walking and running. This condition can cause significant discomfort and impairment in mobility. In this blog post, we will delve into the causes, symptoms, grading of severity, treatments, and management strategies for PTT.
Causes of Posterior Tibial Tendinopathy
PTT typically develops due to a combination of factors, rather than a single cause. Some common causes and contributing factors include:
-
Overuse or Repetitive Stress: Activities that place excessive strain on the posterior tibial tendon, such as running, jumping, or walking on uneven surfaces, can lead to PTT.
-
Age and Degeneration: As we age, tendons naturally weaken and become more susceptible to injury and degeneration. This is a common factor in the development of PTT.
-
Foot Structure: Abnormal foot structures, such as flat feet (pes planus), can increase the risk of PTT by altering the mechanics of the foot and the way forces are distributed.
-
Poor Footwear: Inappropriate or unsupportive footwear can contribute to the development of PTT by not providing adequate arch support.
Symptoms of Posterior Tibial Tendinopathy
Recognizing the symptoms of PTT is essential for early diagnosis and treatment. Common symptoms include:
-
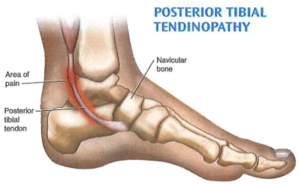
Pain along the inner aspect of the ankle and foot, especially during activity.
-
Swelling on the inside of the ankle.
-
Increased discomfort when standing on tiptoes or attempting to raise the arch of the foot.
-
Weakness in the affected leg, making it difficult to perform activities that involve the posterior tibial tendon.
Grading of Severity
PTT can be classified into different grades of severity based on the extent of tendon damage and functional impairment:
-
Grade I: Mild PTT involves minor tendon inflammation without significant structural damage. Symptoms may include occasional pain and swelling.
-
Grade II: Moderate PTT involves more noticeable tendon damage and dysfunction. Pain and swelling are usually present during physical activities.
-
Grade III: Severe PTT is characterized by significant tendon degeneration, resulting in chronic pain, instability, and difficulty with walking.
Treatments and Management
The treatment and management of PTT can vary depending on the severity of the condition, but here are some common approaches:
-
Rest and Immobilization: For mild cases (Grade I), resting the affected foot and using a walking boot or brace to immobilize the ankle may be sufficient to allow the tendon to heal.
-
Physical Therapy: Physical therapy can help improve the strength and flexibility of the affected leg, as well as address gait abnormalities and posture issues that contribute to PTT.
-
Orthotic Devices: Custom or over-the-counter orthotic inserts can provide additional arch support, improving foot mechanics and reducing strain on the posterior tibial tendon.
-
Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) can help manage pain and reduce inflammation.
-
Corticosteroid Injections: In some cases, corticosteroid injections may be recommended to reduce inflammation and pain.
-
Surgery: For severe cases (Grade III) that do not respond to conservative treatments, surgical intervention may be necessary to repair or reconstruct the damaged tendon.
-
Lifestyle Modifications: Maintaining a healthy weight, wearing supportive footwear, and avoiding activities that exacerbate symptoms can help manage PTT in the long term.
-
Isometric Exercises:
- Both Types of Tendinopathy: Isometric exercises play a crucial role in pain management and loading without worsening symptoms. These exercises engage muscles without causing tendon movement, aiding in pain relief and maintaining muscle strength.
- Holding the top position of a calf raise can reduce pain, warm-up the tendon and be a great starting point for strengthening that is essential for long-term improvement (try 3 sets of 25 to 30 seconds)
- Shockwave Therapy – this can be a great adjunctive therapy to improve pain and reduce nerve sensitisation, promote collagen regeneration of healthy tissue and enhance blood flow and circulation. It is ideal for more chronic tendinopathies such as those that have been around for 3-6 months or longer.

Posterior Tibial Tendinopathy is a condition that can have a significant impact on an individual’s mobility and quality of life. Understanding its causes, recognizing the symptoms, and seeking appropriate treatment and management strategies are essential steps in addressing this condition. Early intervention and a holistic approach to care can help individuals regain function and reduce pain associated with PTT, allowing them to lead a more active and fulfilling life.
Book in today for an assessment if you have been dealing with posterior tibial tendinopathy